Unlike
many diseases, which involve germs, cancer cells are natural body
cells which behave abnormally. They don't perform any beneficial
functions and they can grow rapidly, causing tumors which interfere
with the normal functions of the body. A single cancer cell
can grow into a tumor or metastasize, sending cancer cells to other
locations in the body, where they can grow into tumors. The
challenge in trying to eliminate cancerous cells from our bodies is
that we need to kill every one of them - however, since they are a
part of our body, it is difficult to target only those cells. To
accomplish that task, current medical technology offers us surgery,
chemotherapy, and radiation therapy (also called radiotherapy),
and a number of other treatments which are classified as biologic
response modifiers. Unlike
many diseases, which involve germs, cancer cells are natural body
cells which behave abnormally. They don't perform any beneficial
functions and they can grow rapidly, causing tumors which interfere
with the normal functions of the body. A single cancer cell
can grow into a tumor or metastasize, sending cancer cells to other
locations in the body, where they can grow into tumors. The
challenge in trying to eliminate cancerous cells from our bodies is
that we need to kill every one of them - however, since they are a
part of our body, it is difficult to target only those cells. To
accomplish that task, current medical technology offers us surgery,
chemotherapy, and radiation therapy (also called radiotherapy),
and a number of other treatments which are classified as biologic
response modifiers. |
Surgery |
 The
first step in treating Mo's tumor was surgery. Once we discovered
his tumor, he was scheduled for surgery asap, which turned out to
be the next morning. Thankfully, the tumor was completly removed. Later
in the week, we received the pathology report, which determined what
type of tumor he had - unfortuately it was a Medulloblastoma, which
is malignant. The day after surgery, Mo received another MRI
and then about ten days later he was given a spinal tap. Thankfully,
neither of these test detected any cancer cells in his body. The
results of these tests influenced the initial treatments which included
both the chemotherapy and radiotherapy. The
first step in treating Mo's tumor was surgery. Once we discovered
his tumor, he was scheduled for surgery asap, which turned out to
be the next morning. Thankfully, the tumor was completly removed. Later
in the week, we received the pathology report, which determined what
type of tumor he had - unfortuately it was a Medulloblastoma, which
is malignant. The day after surgery, Mo received another MRI
and then about ten days later he was given a spinal tap. Thankfully,
neither of these test detected any cancer cells in his body. The
results of these tests influenced the initial treatments which included
both the chemotherapy and radiotherapy.
 Over
the course of July and August 2003, we discovered that Mo's tumor
was growing again. This is a recurrence. Fortunately,
it was only growing in a single place, and the entire mass (which
was very small), was removed with a second surgery. Again, after
surgery Mo Because of the recurrence, we changed Mo's chemotherapy
to a treatment which allows him to be given different chemotherapy
medicines at higher doses (described below). Over
the course of July and August 2003, we discovered that Mo's tumor
was growing again. This is a recurrence. Fortunately,
it was only growing in a single place, and the entire mass (which
was very small), was removed with a second surgery. Again, after
surgery Mo Because of the recurrence, we changed Mo's chemotherapy
to a treatment which allows him to be given different chemotherapy
medicines at higher doses (described below). |
Chemotherapy |
|  Healthy
cells grow in a well-established pattern, and when they divide,
an identical copy is produced. The body makes only the number
of normal cells that it needs at any given time. As each normal
cell matures, it loses its ability to reproduce and it is also pre-programmed
to die at a specific time. Healthy
cells grow in a well-established pattern, and when they divide,
an identical copy is produced. The body makes only the number
of normal cells that it needs at any given time. As each normal
cell matures, it loses its ability to reproduce and it is also pre-programmed
to die at a specific time.
Tumor cells, on the other hand, reproduce uncontrollably and grow
in an unpredictable way. Chemotherapy involves the use of drugs
that damage rapidly multiplying cells, such as those found in brain
tumors. There are hundreds of chemotherapy drugs and they
use a variety of approaches to destroy cancer cells.
 Unfortunately, some good normal cells are damaged along with the
bad tumor cells. The normal cells which are most often affected
are those which grow and divide rapidly, including cells in the
bone marrow, hair, mouth, and intestines. Hair loss is an example
of a side effect due to damage to “good” cells. Unlike tumor
cells, however, normal cells do repair themselves. Each child
reacts differently to each chemotherapy drug. Some children
experience severe side effects, while others do not. Many
of these side effects can be managed by various control measures.
Unfortunately, some good normal cells are damaged along with the
bad tumor cells. The normal cells which are most often affected
are those which grow and divide rapidly, including cells in the
bone marrow, hair, mouth, and intestines. Hair loss is an example
of a side effect due to damage to “good” cells. Unlike tumor
cells, however, normal cells do repair themselves. Each child
reacts differently to each chemotherapy drug. Some children
experience severe side effects, while others do not. Many
of these side effects can be managed by various control measures.
 Chemotherapeutic agents are chosen based on several characteristics
of the tumor cells. A child’s doctor may select different
drugs to damage the tumor cells in different parts of their life
cycle or to interrupt various cell functions. The frequency
of chemotherapy treatment depends on many factors and the effect
of the chemo medicines on a child’s healthy cells can be a factor
in determining frequency of the treatments.
Chemotherapeutic agents are chosen based on several characteristics
of the tumor cells. A child’s doctor may select different
drugs to damage the tumor cells in different parts of their life
cycle or to interrupt various cell functions. The frequency
of chemotherapy treatment depends on many factors and the effect
of the chemo medicines on a child’s healthy cells can be a factor
in determining frequency of the treatments.
 In order to make the most progress in treating childhood brain tumors,
doctors coordinate their efforts through clinical trials. Clinical
trials, also called studies or protocols, involve designing a particular
treatment program to treat specific types of tumors. Doctors evaluate
these treatments and try to decide how to improve survival rates
and reduce side effects. Each study or protocol builds on
those that have gone before it.
In order to make the most progress in treating childhood brain tumors,
doctors coordinate their efforts through clinical trials. Clinical
trials, also called studies or protocols, involve designing a particular
treatment program to treat specific types of tumors. Doctors evaluate
these treatments and try to decide how to improve survival rates
and reduce side effects. Each study or protocol builds on
those that have gone before it.
 Mo's
initial treatment consisted of radiation and low-dose chemotherapy.
The treatment has been developed over the last 10-15 years.
He completed the radiation part of the treatment, and part
of the chemotherapy. The chemotherapy was planned to last
for about 15 months, which would have ended in Feb. of 2004. Because
his particular tumor did not respond completely to radiation and
low-dose chemotherapy, the chemotherapy treatments were switched
to a treatment which uses high dose chemotherapy followed by stem
cell rescue (described below). Mo's
initial treatment consisted of radiation and low-dose chemotherapy.
The treatment has been developed over the last 10-15 years.
He completed the radiation part of the treatment, and part
of the chemotherapy. The chemotherapy was planned to last
for about 15 months, which would have ended in Feb. of 2004. Because
his particular tumor did not respond completely to radiation and
low-dose chemotherapy, the chemotherapy treatments were switched
to a treatment which uses high dose chemotherapy followed by stem
cell rescue (described below).
 High Dose Chemotherapy
with Stem Cell Rescue High Dose Chemotherapy
with Stem Cell Rescue
 As
mentioned, chemotherapy drugs kill rapidly growing cells, so one
of the limiting factors for the dosage of chemotherapy is how much
damage it will do to healthy cells. Blood is composed of many
different types of cells, each with its own function for maintaining
a healthy body. All blood cells are produced by stem cells,
which are a part of the bone marrow. Because they grow rapidly,
stem cells are vulnerable to chemotherapy drugs and will be killed
when high doses of chemotherapy are given. In order to use
high doses of chemotherapy, stem cells are "harvested"
from the body before chemotherapy begins, and then infused back
into the body after chemotherapy is completed (i.e. they rescue
the body's blood production system). Stem cell rescue allows
us to use very high doses of chemotherapy drugs to attempt to destroy
every cancer cell in a body. As a side effect, almost every
other rapidly dividing cell is killed, leaving the body with very
little resistance to infections. A few days after chemotherapy,
the stem cells which have been harvested and frozen are returned
to the body where they magically find their way back to the bone
marrow ("engraft") and resume blood cell production. It
takes a few weeks for the stem cells to produce enough white blood
cells for the body to fight off infections on its own. While
the blood system is regenerating, the patient has to stay in a relatively
isolated ward in the hospital, with his health closely monitored
and taking IV antibiotics, fluids, and nutrition. As
mentioned, chemotherapy drugs kill rapidly growing cells, so one
of the limiting factors for the dosage of chemotherapy is how much
damage it will do to healthy cells. Blood is composed of many
different types of cells, each with its own function for maintaining
a healthy body. All blood cells are produced by stem cells,
which are a part of the bone marrow. Because they grow rapidly,
stem cells are vulnerable to chemotherapy drugs and will be killed
when high doses of chemotherapy are given. In order to use
high doses of chemotherapy, stem cells are "harvested"
from the body before chemotherapy begins, and then infused back
into the body after chemotherapy is completed (i.e. they rescue
the body's blood production system). Stem cell rescue allows
us to use very high doses of chemotherapy drugs to attempt to destroy
every cancer cell in a body. As a side effect, almost every
other rapidly dividing cell is killed, leaving the body with very
little resistance to infections. A few days after chemotherapy,
the stem cells which have been harvested and frozen are returned
to the body where they magically find their way back to the bone
marrow ("engraft") and resume blood cell production. It
takes a few weeks for the stem cells to produce enough white blood
cells for the body to fight off infections on its own. While
the blood system is regenerating, the patient has to stay in a relatively
isolated ward in the hospital, with his health closely monitored
and taking IV antibiotics, fluids, and nutrition.
| Mo's treatments are as follows (dates are approximate): |
 |
1. Stem
cell mobilization and harvest |
 |
 |
Under normal conditions, stem cells
reside in the bone marrow where they can be harvested by poking
a pelvic bone needle into the pelvic bone and extracting them.
An easier and less painful way to harvest them is by attempting
to force them into the bloodstream ("mobilization")
where they can then be extracted directly from the blood using
a centrifuge. In order to encourage Mo's stem cells to
move out of his bone marrow and into his blood, a combination
of chemotherapy along with a medicine to encourage stem cell
growth (a "growth factor") are used. On 9/18
Mo was given a dose of chemotherapy and he is being given the
growth factor every day for a week or so. During the week
of 9/29 Mo's blood will be tested to see if it is feasible to
extract stem cells. Radiation treatments make it more
difficult to mobilize the stem cells into the blood, so the
fact that Mo had radiotherapy decreases the likelihood that
stem cells can be harvested from his blood. If they can't
be harvested from his blood, they will be harvested from his
pelvic bones with a needle. Harvesting stem cells from
the bones takes place in a surgical suite under anesthesia and
Mo would be uncomfortable for a couple days afterwards. |
 |
2. Chemotherapy |
 |
 |
On 10/13 Mo will be admitted to the hospital
for the high dose chemo/stem cell rescue procedure.
Day
1: he will just settle in.
Day
2 - 4: he will be given a single chemotherapy medicine.
Day 5-7: he will b:e given
two other chemotherapy drugs.
Day
8-10: he will be given a rest. |
| |
3. Stem cell rescue |
| |
|
Day 11: his stem cells
will be put back into his body ("infused"). They
will find their way back to the bone marrow and start producing
blood cells.
Next 4-5 weeks:
Mo's blood counts will continue to drop for a week or so, then
they will recover. He will remain in the hospital during
this time where his health will be carefully monitored. He
will require quite a bit of medication (as well as IV fluids
and nutrition) during the first few weeks after the reintroduction
of his stem cells.
Next couple
of months: When his blood counts are high enough,
he will be able to come back home, but he will not be able to
go to crowded places (school, malls, movies, etc.) until his
resistance to disease is pretty much back to normal - this will
probably take a couple of months. |
|
| 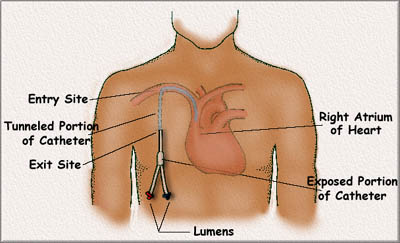
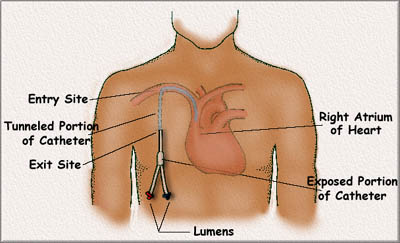
Pheresis Catheter Illustration. Taken from the
web and modified.
Mo's catheter is actually on his left side.
 For
this part of his treatment, Mo will require medicines, fluids,nutrition,
contrast dyes, and blood to be administered intravenously. In
order to avoid the pain and stress of inserting needles into his
veins for each of these procedures, Mo has a pheresis catheter implanted
under his skin in his chest. The pheresis catheter consists
of a two-chambered tube (divided longitudinally down the middle)
which runs from one of the major ateries of the heart out of his
chest where it divides into two lumens . Each time Mo receives
fluids, the medical staff will use the pheresis catheter, which
is much better than trying to stick an IV needle into his veins
every time. For
this part of his treatment, Mo will require medicines, fluids,nutrition,
contrast dyes, and blood to be administered intravenously. In
order to avoid the pain and stress of inserting needles into his
veins for each of these procedures, Mo has a pheresis catheter implanted
under his skin in his chest. The pheresis catheter consists
of a two-chambered tube (divided longitudinally down the middle)
which runs from one of the major ateries of the heart out of his
chest where it divides into two lumens . Each time Mo receives
fluids, the medical staff will use the pheresis catheter, which
is much better than trying to stick an IV needle into his veins
every time.
|
Biologic Response Modifiers |
 We
are also considering the use of a "differentiating agent"
which is a medicine classified as a biologic response modifier. This
drug, which is related to hair growth and acne medicines, is used
to try to force cancer cells to "differentiate", which is
to transform themselves into normal types of tissue rather than remaining
in their primitive state and multiplying rapidly. I will describe
this further if we end up using it. We
are also considering the use of a "differentiating agent"
which is a medicine classified as a biologic response modifier. This
drug, which is related to hair growth and acne medicines, is used
to try to force cancer cells to "differentiate", which is
to transform themselves into normal types of tissue rather than remaining
in their primitive state and multiplying rapidly. I will describe
this further if we end up using it. |
Radiation |
Mo'd initial treatment included the
use of radiation therapy to try to destroy any tumor cells left
behind after surgery. He completed his radiation treatments
at the end of February, 2003.
How Radiation Therapy Works
Radiation treatments or radiotherapy directs high-energy x-rays
at targeted areas of the body to destroy tumor cells. Many
brain tumors are radiosensitive, which means that the cancer cells
can be destroyed by radiation therapy. The challenge to using radiation
is to deliver it in such a way that it does minimal damage to healthy
cells and maximum damage to tumor cells. There is also a limit
to the amount of radiation an individual can receive in his or her
lifetime, so doctors are careful in determining dosage and total
amounts to be given.
 What Makes
Brain Tumors Radiosensitive What Makes
Brain Tumors Radiosensitive
Rapidly dividing cells in tumors have unstable DNA (the material
in the cell that tells it how to grow). This DNA is susceptible
to damage from ionizing radiation. Normal cells can also be damaged,
but they can repair themselves. The repair mechanisms of cancer
cells are not very effective, so cancer cells tend to not grow back.
 Mo's Treatments Mo's Treatments
Mo's radiotherapy was divided into 2 parts, which were administered
daily, excluding weekends. During the first part, he was given
13 treatments to his head and spine ("cranial-spinal radiation
"). During the second part, called the "boost",
he was given 18 treatments to the area of the brain where the tumor
was removed (the posterior fossa).
|

 Radiation is administered
with a linear accelerator. The linear accelerator can be
rotated to deliver the radiation from various angles to carefully
and precisely target the area of the body receiving the radiation,
thus minimizing "scatter", which is exposure to areas of
the body which don't need to be irradiated. The treatments
required Mo to lie on a bench and remain as still as possible, sometimes
when he was very uncomfortable. Radiation is administered
with a linear accelerator. The linear accelerator can be
rotated to deliver the radiation from various angles to carefully
and precisely target the area of the body receiving the radiation,
thus minimizing "scatter", which is exposure to areas of
the body which don't need to be irradiated. The treatments
required Mo to lie on a bench and remain as still as possible, sometimes
when he was very uncomfortable. |

One of the linear accelerators Mo used at the University
of Wisconsin Hospital. On the bed are the foam body mold and
plastic-mesh head mold which were used to help him maintain his position
during the cranial-spinal treatments. |
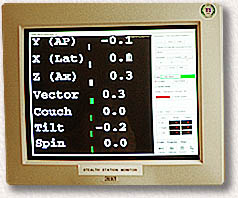
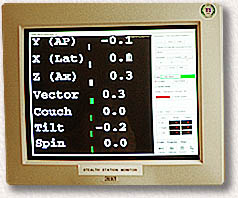
The IMRT setup can control the position of the
x-ray beam to within one-tenth of a mm and one-tenth of a degree!
|
| The treatments were very carefully planned
to focus the radiation on the target areas of Mo's body. During
the 2nd part of his treatment (the boost to the tumor bed), his doctors
used IMRT, a technique which allows them to deliver the radiation
with an accuracy of about 1/2 of a millimeter, minimizing exposure
to other areas of his brain. For the IMRT, the doctors used
MRI and CT scans to create a 3 dimensional map of part of his brain,
and then used a device which allowed them to conduct real-time tracking
of the location of Mo's brain relative to the X-ray beam during treatments.
In order to take advantage of this technique, Mo had to lie
very still, as even a yawn or a sneeze would change his position on
the machine! |
Sources:
Shiminski-Maher, Cullen, Sansalone, Childhood
Brain and Spinal Cord Tumors, O'Reilly - Sebastopol, CA, Jan.
2002.
Blood and Marrow Stem Cell Transplantation,
The Leukemia and Lymphoma Society - White Plains, NY
Further Reading:
 For
anyone wanting more insight than is being provided on our website,
there is a lot of info on the web. As a recommendation, you might
look at Understanding
and Coping with Your Child's Brain Tumor, which is published
by the National Brain Tumor Foundation. It requires the Acrobat
Reader, which probably already on your computer (it should open
automatically if you click the link). It is well written and
not-too-technical. In particular, there are sections on chemo
and radiation. For
anyone wanting more insight than is being provided on our website,
there is a lot of info on the web. As a recommendation, you might
look at Understanding
and Coping with Your Child's Brain Tumor, which is published
by the National Brain Tumor Foundation. It requires the Acrobat
Reader, which probably already on your computer (it should open
automatically if you click the link). It is well written and
not-too-technical. In particular, there are sections on chemo
and radiation.
 Dr.
Roger Packer is, one of the world's foremost experts on medulloblastoma.
He developed the initial radiation/chemotherapy protocol that
Maurice, and most other medulloblastoma patients undergo. There
is a reasonably non-technical paper about medulloblastoma, written
by Dr. Packer, here. Dr.
Roger Packer is, one of the world's foremost experts on medulloblastoma.
He developed the initial radiation/chemotherapy protocol that
Maurice, and most other medulloblastoma patients undergo. There
is a reasonably non-technical paper about medulloblastoma, written
by Dr. Packer, here. |
|